Hypothyroidism: Overview
Alternative names: Underactive thyroid gland
Hypothyroidism is a condition in which the thyroid gland does not make sufficient thyroid hormone to meet the body's requirements. Caused in almost all cases by autoimmune disease, the result is that the immune system goes awry and begins gradually to destroy the thyroid gland. This process is not usually associated with thyroid gland discomfort but may cause the gland to enlarge or shrink in size.
- understand what's happening to your body
- learn what you should be doing right now
- identify any nutritional deficiencies
There are three types of hypothyroidism:
- Primary hypothyroidism: The most common type, in which the thyroid doesn't produce enough thyroid hormone.
- Secondary hypothyroidism: Occurs when the pituitary gland does not release enough of thyroid-stimulating hormone (TSH) that prompts the thyroid to manufacture thyroid hormone.
- Tertiary hypothyroidism: Results from a malfunction of the hypothalamus, the part of the brain that controls the endocrine system.
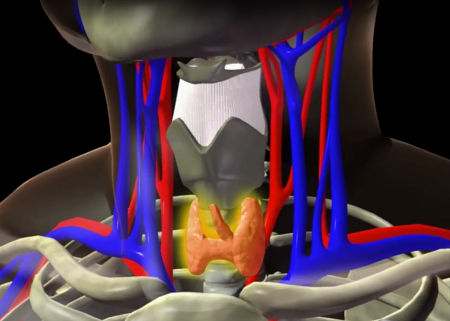
The thyroid gland is located at the lower front of the neck and produces and stores hormones that are essential for the function of every cell in the body. These hormones help regulate the heart rate, blood pressure, body temperature, oxygen usage, digestion, neuromuscular function, metabolism, and growth.
Hypothyroidism is one of the most common chronic diseases. It occurs when the thyroid gland fails to produce or secrete as much thyroxine (T4) and triiodothyronine (T3) as the body needs. About 14-20 times as much T4 as T3 is normally produced; T4 contains four iodine atoms, and is converted to the more active T3 form (with three iodine atoms) in the liver, brain, and other tissues. Selenium and zinc play crucial roles in this conversion process, so any deficiency can cause a conversion problem.
Incidence; Causes and Development; Contributing Risk Factors
Hypothyroidism is relatively common. It affects between 1 in 100 to 3 in 100 women of child-bearing age. It is more common in women than in men, and it becomes more common with age. Hypothyroidism occurs in up to 5 to 10% of older women; up to 20% of women over 60 have evidence of hypothyroidism.
Hypothyroidism is usually caused by an autoimmune disease (Hashimoto's thyroiditis), but may also be caused by radiation therapy, thyroid surgery, or certain medications.
Another common cause of hypothyroidism is the treatments used for hyperthyroidism (overactive thyroid), namely radioactive iodine or anti-thyroid medications. These often lead to permanent failure of the thyroid gland after a number of years. Approximately 50% of patients treated with radioiodine, and many treated with antithyroid drugs, eventually develop hypothyroidism and should be tested about once a year.
Less common causes of Hypothyroidism include:
- Inherited thyroid disease (defective or non-existent thyroid gland)
- Iodine deficiency
- Pregnancy
- Pituitary gland disorder, whereby it does not produce sufficient thyroid stimulating hormone
Hypothyroidism tends to run in families. If you have a history of either hypothyroidism, or paradoxically, hyperthyroidism in your family, it increases the chance that you may someday develop the condition. However, except for a few rare disorders, hypothyroidism is not transmitted in a typical dominant or recessive manner. If you have a strong family history of underactive or overactive thyroid disease, you should mention this to your physician.
Signs and Symptoms
Symptoms may not appear until years after the thyroid has stopped functioning, and they are often mistaken for signs of other illnesses, or menopause, or aging.
Hypothyroidism slows metabolism and affects essentially every system in the body. Symptoms include generalized fatigue, weight gain, thinning (brittle) hair, dry scaly skin, thin nails that break easily, constipation, alterations in menses, aching muscles, and slow heart rate. You may notice changes in behavior, such as decreased ability to concentrate, reading and calculating are more difficult, and you may experience decreased interest in personal relationships or work. Hypothyroidism can cause or worsen depression.
Other symptoms include loss of appetite, painful pre-menstrual periods, muscle weakness, a yellow-orange coloration in the skin (particularly on the palms), yellow bumps on the eyelids, hair loss (including eyebrows), recurrent infections, depression, slow speech, lowering of the voice, premature aging and drooping swollen eyes.
Diagnosis and Tests
Hypothyroidism is more common than is typically diagnosed. It is possible to have some laboratory values be returned in the normal range when you have low thyroid symptoms. Oral temperatures during the day of less than 98.0°F (36.7°C) are very suspicious.
Diagnosis involves a simple blood test which measures your thyroid hormone (thyroxine or T4) and TSH (Thyroid-stimulating hormone) levels. An elevation of TSH is a very sensitive index of reduced thyroid function. Somewhat like the thermostat in your home, when thyroid hormone levels fall, TSH (the furnace) is switched on to stimulate the thyroid gland. When thyroid hormone levels are low for a long time, TSH levels remain high. Thus, hypothyroidism is characterized by a TSH level that is above the normal range and a thyroxine level that is below or at the low end of the normal range (everyone's set point is a little different). Your physician can assist in the interpretation of these results, or you may wish to see a physician (an Endocrinologist) who specializes in hormonal disorders.
Some patients with hypothyroidism have problems converting T4 to T3. Unfortunately, many doctors don't address this problem, and some won't even look at the T3 levels on a blood test, whereas others will prescribe synthetic T3 or natural thyroid hormone. The bottom line is that few doctors will try to find the underlying cause of any T4-to-T3 conversion problem, which should be the goal of any effective natural treatment protocol. The answer may be a simple and easily-correctable mineral deficiency such as selenium or zinc.
Treatment and Prevention
A medication called L-Thyroxine (L-T4) is used to replace the missing thyroid hormone. Some preparations also include a second form of thyroid hormone, tri-iodothyronine (L-T3). These hormones are chemically identical to those made by your own thyroid gland. Consequently, when the correct doses are prescribed and restore your metabolism to normal, the treatment is not accompanied by side-effects. The medication is in the form of a tablet, taken once a day. Taking too much thyroid hormone will, of course, speed up metabolism and can cause rapid or irregular heart rate and loss of calcium from the bone. However, excess thyroid hormone levels are unlikely to occur when the treatment is carefully prescribed and monitored.

When hypothyroidism is diagnosed, most doctors will prescribe thyroid medication and many use Synthroid (T4). However, a recent blinded study demonstrated that T4 and T3 in combination produced greater benefits than T4 alone, especially in the area of mental functioning.
Hypopituitarism (low functioning pituitary) and hypothyroidism (low functioning thyroid) can both result in deficient production of T4, which is the raw material the body uses to produce the active thyroid hormone T3. Your doctor should be able to help determine which medications are best for you.
The treatment of choice preferred by conventional doctors is T4 (Synthroid) because of its long half-life in the body (which helps provide steady T3 levels), once-a-day administration, and effectiveness in the treatment of such cases. Patients with hypopituitarism and hypothyroidism may, however, suffer with Wilson's Syndrome at the same time. In such cases, T4 therapy may not be adequate because impaired conversion of the T4 to the active compound T3 may prevent sufficient normalization of body temperature patterns and, in some cases, can even feed the vicious cycle of Wilson's Syndrome. The simultaneous use of T4 with T3 may be the best approach for hypothyroidism, especially if Wilson's Syndrome is suspected. Many doctors prefer using the standard T4/T3 combination found in desiccated thyroid products such as Armour thyroid and other generic brands. Additional adjustments in the T4/T3 ratio can be made to meet the needs of individual patients.
Aside from taking a daily tablet, containing L-thyroxine, you should not have to change your lifestyle.
Is there a way to prevent hypothyroidism? Iodine deficiency can cause hypothyroidism but this is very unlikely in North America where the iodine supply is abundant. There are no other preventative measures you can take to avoid hypothyroidism.
Prognosis; Complications
The underlying cause of hypothyroidism is not reversible. However, the consequences of hypothyroidism can be treated very effectively by taking thyroid hormone replacement medication. The dose of thyroid hormone can be carefully regulated so that your body's metabolism is restored to normal. You should have your blood tested at least once a year, or more often if necessary, to be certain that the thyroid hormone dose you are taking is satisfactory.
Recognition and proper daily treatment of low thyroid function using thyroid hormone replacement therapy will result in resolution of deficiency symptoms usually beginning within the first month of therapy and reaching a maximum at 6-12 months of treatment. Nevertheless, it is probable that the patient will require thyroxine replacement for the rest of his or her life.
Problems with the thyroid can be the cause of many recurring illnesses and fatigue. Hypothyroidism can cause:
- Goiter
- Heart disease
- Depression and slowed mental functioning
- Infertility
- Birth defects
- Peripheral neuropathy
- Carpal tunnel syndrome
- Raynaud's phenomenon
- Myxedema
- Digestive problems: hydrochloric acid production is reduced, resulting in malabsorption of nutrients, undigested proteins, and digestive complaints
- Significantly increased cholesterol and homocysteine levels: it is implicated in about 10% of patients with high cholesterol levels
Correcting hypothyroidism can lead to a 30% drop in cholesterol and homocysteine levels.
Signs, symptoms & indicators of Hypothyroidism:
Lab Values - Cells
Lab Values - Common
Lab Values - Hormones
Lifestyle
Symptoms - Bowel Movements
Symptoms - Environment
Symptoms - Food - General
Symptoms - General
Symptoms - Glandular
 Possible/minor/major swelling at front of neck
Possible/minor/major swelling at front of neck
A goiter is a common symptom of hypothyroidism / too little iodine in the diet.
Symptoms - Hair
Symptoms - Head - Eyes/Ocular
 Bags under eyes
Bags under eyes
People suffering from a thyroid problem (usually underactive, sometimes overactive) may have very baggy eyes.
Symptoms - Head - Mouth/Oral
Symptoms - Head - Nose
Symptoms - Metabolic
Symptoms - Mind - Emotional
Symptoms - Mind - General
Symptoms - Muscular
Symptoms - Nails
 Brittle fingernails
Brittle fingernails
Thyroid diseases may produce brittle nails or splitting of the nail bed from the nail plate.
Symptoms - Nervous
Symptoms - Reproductive - Female Cycle
Symptoms - Reproductive - General
Symptoms - Skeletal
Symptoms - Skin - General
Symptoms - Sleep
Conditions that suggest Hypothyroidism:
Circulation
 Coronary Disease / Heart Attack
Coronary Disease / Heart Attack
The thyroid affects every organ in the body, including the heart. Almost any type of heart disease can be worsened by thyroid disorder, so thyroid function should always be checked if cardiac symptoms are worsening. Hypothyroidism weakens the heart muscle in both its contraction and relaxation phases, resulting in less blood being pumped. And, because the heart muscle does not relax normally in between beats, a potentially serious condition called diastolic dysfunction may result.
 Hypertension (High Blood Pressure)
Hypertension (High Blood Pressure)
Hypothyroidism reduces the amount of nitric oxide in the lining of the blood vessels, causing them to stiffen, which in turn raises diastolic blood pressure.
 Megaloblastic Anemia / Pernicious Anemia
Megaloblastic Anemia / Pernicious Anemia
Pernicious anemia is associated with other autoimmune conditions such as Hashimoto's disease, a form of hypothyroidism.
 Anemia
Anemia
If anemia is identified as a problem then the likelihood of Hypothyroidism is reduced. Therefore, it is wise to rule out anemia first, because both can contribute to similar symptomology. Of course, it is not impossible for both to occur simultaneously, but this is less likely.
Digestion
 Heartburn / GERD / Acid Reflux
Heartburn / GERD / Acid Reflux
Gastrointestinal manifestations of hypothyroidism include GERD as a result of delayed emptying of the stomach.
Eyes / Ocular
 Retinitis Pigmentosa
Retinitis Pigmentosa
There is an increased occurrence of thyroid disease (Hashimoto's thyroiditis) in patients with retinitis pigmentosa. [ Am J Ophthalmol, 1996 Dec, 122:6, pp.903-5 Abstract]
Female-Specific
 Amenorrhea
Amenorrhea
In many cases, an underactive or overactive thyroid gland is responsible for the absent menstrual cycles.
 Female Infertility
Female Infertility
Hypothyroidism in women sometimes causes ovarian problems; ovulation may become less frequent or disappear altogether.
Glandular
Hormones
Infections
Inflammation
Lab Values
Male-Specific
 Male Infertility (Low Sperm Count)
Male Infertility (Low Sperm Count)
The thyroid gland is responsible for balancing cell metabolism, so when the thyroid gland is not functioning properly, cell metabolism suffers. This causes changes in the production of sperm.
Mental
Metabolic
 Hypoglycemia
Hypoglycemia
Patients suffering with Wilson's Syndrome, a form of hypothyroidism, occasionally experience intense and previously unfamiliar cravings for sweets. The low body temperature patterns may affect the function of enzymes involved in glucose metabolism that could result in lower blood sugar levels which might contribute to sweet cravings.
Musculo-Skeletal
 Rheumatoid Arthritis
Rheumatoid Arthritis
A study of rheumatoid arthritis patients found evidence of thyroid dysfunction 3 times more often than in controls. The excess thyroid dysfunction was due to either hypothyroidism or Hashimoto's thyroiditis. [Annals of Rheumatic Diseases, 1993;52 pp.454-6]
 Osteoporosis - Osteopenia
Osteoporosis - Osteopenia
People with hypothyroidism can develop osteoporosis if they are taking too much thyroid hormone.
Reproductive
Skin-Hair-Nails
 Male Hair Loss
Male Hair Loss
In rare cases, diffuse hair loss may be the only symptom of hypothyroidism, but in many people with hypothyroidism the hair is not affected. Once thyroid hormone is administered, regrowth of hair occurs in approximately 2 months.
Sleep
 Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA)
Hypothyroidism can present itself as obstructive sleep apnea and snoring.
Symptoms - Glandular
Risk factors for Hypothyroidism:
Diet
 Vegan Diet Consequences
Vegan Diet Consequences
Sub-clinical hypothyroidism, with raised thyroid stimulating hormone (TSH) levels but mild or absent overt symptoms, has been found to be more common among vegans than the general population. Most vegans have low iodine intakes but a significant minority consume excessive amounts of iodine from seaweed, particularly kelp. Both low and excessively high iodine intakes in vegans have been linked to elevated TSH levels. The optimal range for TSH appears to be 1-2 mIU/l with values below 0.5 suggesting hyperthyroidism and values above 5 suggesting hypothyroidism.
Family History
 Hypothyroidism in family members
Hypothyroidism in family members
Hypothyroidism tends to "run in families". If you have a history of either hypothyroidism, or paradoxically, hyperthyroidism in your family, it increases the chance that you may someday develop the condition. However, except for a few rare disorders, hypothyroidism is not transmitted in a typical dominant or recessive manner. If you have a strong family history of underactive or overactive thyroid disease, you should mention this to your physician.
 Hyperthyroidism in family members
Hyperthyroidism in family members
A family history of hyperthyroidism leads to a higher chance of developing hypothyroidism (not just hyperthyroidism).
Glandular
Hormones
 Progesterone Low or Estrogen Dominance
Progesterone Low or Estrogen Dominance
Progesterone increases sensitivity of estrogen receptors, and can therefore redirect estrogen activity and inhibit many of unopposed estrogen's undesirable side-effects, which includes interference with thyroid hormone activity.
Lab Values - Chemistries
Nutrients
 Copper Deficiency
Copper Deficiency
There are a limited number of studies that suggest low copper levels may reduce thyroid function. In cases where hypothyroidism is not responding properly to medication, make sure that copper levels are normal.
Supplements, Medications, Drugs
Symptoms - Food - General
Symptoms - Food - Intake
 High iodine consumption
High iodine consumption
Amongst adults, low iodine intake or very high intakes can cause hypothyroidism. Excessive iodine has a complex disruptive effect on the thyroid and may cause hypothyroidism in susceptible individuals.
Hypothyroidism can lead to:
Skin-Hair-Nails
 Female Hair Loss
Female Hair Loss
In rare cases, diffuse hair loss may be the only symptom of hypothyroidism, but in many people with hypothyroidism the hair is not affected. Once thyroid hormone is administered, regrowth of hair occurs in approximately 2 months.
Hypothyroidism could instead be:
Environment / Toxicity
 Fluoride Toxicity
Fluoride Toxicity
Though apparently vague and non-specific, most of the symptoms of fluoride toxicity point towards some kind of profound metabolic dysfunction, and are strikingly similar to the symptoms of hypothyroidism.
Mental
 Schizophrenia
Schizophrenia
The book Natural Healing for Schizophrenia reports that 10% of patients diagnosed with "schizophrenia" have been found to have thyroid imbalances.
Recommendations for Hypothyroidism:
Botanical / Herbal
 Ginger Root
Ginger Root
The liberal use of ginger, cayenne and other spicy herbs has helped restore a normal body temperature for some people with hypothyroidism.
 Bladderwrack
Bladderwrack
People living near oceans or seas have a historically low rate of hypothyroidism that is due, in part, to ingestion of iodine-rich food, such as seafood and seaweeds like bladderwrack. Either hypothyroidism or goiter due to insufficient intake of iodine may possibly improve with bladderwrack supplementation, though human studies have not confirmed this at the time of writing.
Diet
 Raw Food Diet
Raw Food Diet
A short-term (2-4 week) diet of only raw foods, with heavy emphasis on raw greens, seaweed, nuts, seeds, sprouted beans and seeds, and freshly extracted vegetable juices, can improve thyroid function. Although a long-term raw food diet may help you feel warmer, many raw foodists find they tend to be cold.
Hormone
 Natural Progesterone
Natural Progesterone
Within weeks of using adequate natural progesterone cream, symptoms of hypothyroidism may disappear. This is because natural progesterone increases sensitivity of estrogen receptors, and can therefore redirect estrogen activity and inhibit many of unopposed estrogen's undesirable side-effects, which include interference with thyroid hormone activity.
Laboratory Testing
 Test Adrenal Function
Test Adrenal Function
Cortisol and DHEA are among the hormones produced by the adrenal glands. It is possible that these hormones can reduce the immune system dysfunction seen in Hashimoto's thyroiditis. More studies are needed, but taking these medications appropriately carries little (if any) risk and can markedly improve the patient's function and overall health.
Mineral
 Iodine
Iodine
Sometimes a low functioning thyroid gland will improve with the addition of iodine in some form. Seaweeds and kelp have been found helpful. See link between hypothyroidism and selenium. Excessive iodine ingestion can cause either hypothyroidism or hyperthyroidism and should be avoided.
 Selenium
Selenium
Selenium and iodine are two minerals which are important in the proper functioning of the thyroid. While the importance of iodine has been known for a long time, the importance of selenium has only been discovered and explored since 1990.
The following is a summary of the possible interactions of selenium and iodine to consider when dealing with thyroid abnormalities:
- A selenium deficiency causes an iodine deficiency to worsen
- When both are deficient, giving selenium alone results in a worsening of existing hypothyroidism
- If iodine intake is low, selenium intake should also be kept low or the two should be supplemented together
- If iodine intake is high and selenium is low, the thyroid may over-produce thyroid hormone (Grave's hyperthyroidism), the thyroid can be damaged from oxidation and hypothyroidism may result (Hashimoto's thyroiditis)
The solution to nutrient supplementation for hypothyroidism may be to take both selenium and iodine simultaneously and gradually increase the dose. A good recommendation may be to start with 100mcg of selenium and 1 kelp tablet per day and gradually work up to 400-600mcg of selenium and 2-4 tablets of kelp per day.
Click to see sample report
Your body is a highly complex, interconnected system. Instead of guessing at what might be wrong, let us help you discover what is really going on inside your body based on the many clues it is giving.
Our multiple symptom checker provides in-depth health analysis by The Analyst™ with full explanations, recommendations and (optionally) doctors available for case review and answering your specific questions.
KEY














