Hyperthyroidism: Overview
Alternative names: Overactive Thyroid, Thyrotoxicosis
Hyperthyroidism occurs when the thyroid gland produces too much thyroid hormone. Left untreated, hyperthyroidism can lead to serious heart problems, bone problems, or (rarely) thyroid storm, which is a medical emergency.
- let The Analyst™ find what's wrong
- have a doctor review your case (optional)
- identify any nutritional deficiencies
The thyroid gland is shaped like the letter "U". The larger side parts are tucked in behind neck muscles next to the trachea (windpipe) while the middle connecting part is closer to the skin, just below the larynx (Adam's apple). It is like two walnuts connected at the bottom by an almond. The normal thyroid gland is barely palpable by a physician's hand, and then it is only the connecting part that can be felt. Enlargement of the gland occurs with most thyroid ailments and is either generalized (a goiter), nodular (bumpy), or both.
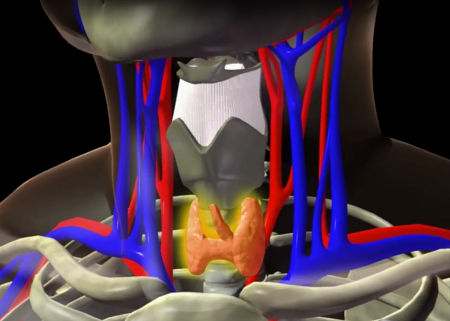
The sole function of the thyroid gland is to make thyroid hormone. The production process involves uptake of iodine from the bloodstream and attachment of this mineral to a protein produced within the gland. Production and release of thyroid hormone by the thyroid gland are controlled by another gland – the pituitary. Located at the base of the brain, the pituitary gland senses the body's need for thyroid hormone and then triggers the thyroid gland by releasing a chemical named thyroid stimulating hormone, or TSH. Because of this close relationship, disease of the pituitary can affect function of the thyroid gland.
Thyroid hormone is the body's 'governor'. It controls the rate of metabolism – the speed of physiologic processes and functions. Under normal circumstances everything is fine-tuned: The thyroid and its pituitary controller keep the body's machinery running at the most effective and efficient rate. But a host of environmental and genetic factors can foul the system.
The most common disease of the thyroid gland is hypothyroidism, or underactive thyroid. With too little thyroid hormone, the machinery slows and the person slows. Fatigue, somnolence, mental sluggishness, and a desire for high room temperature are common symptoms. In advanced states the victim has thickened and boggy facial skin, a slow raspy voice, baggy eyes and a dull appearance. Thinking is slowed, and the person may appear depressed or even confused. Because an underactive thyroid gland develops slowly, the problem often goes unrecognized by the patient, the family and even the physician. Too often the trouble is attributed to old age. Diagnosis is easy if a blood test is obtained. And treatment with a daily thyroid hormone tablet is also easy.
Incidence; Causes and Development
The leading cause of hyperthyroidism is Graves' disease. Graves' disease represents a basic defect in the immune system, causing production of immunoglobulins (antibodies) which stimulate and attack the thyroid gland, causing growth of the gland and overproduction of thyroid hormone. Similar antibodies may also attack the tissues in the eye muscles and in the skin on the front of the lower leg.
- Graves' disease occurs in less than 1⁄4 of 1% of the population
- Graves' disease is 8 times more prevalent among women than men
- Graves' disease usually occurs in middle age, but can occur at any age
- Graves' disease is not curable, but it is a very treatable disease
- Some 3% to 4% of those without symptoms have suppressed TSH levels suggestive of subclinical Graves' disease.
There are several elements contributing to the development of Graves' disease. There is a genetic predisposition to autoimmune disorders and infections and stress play a part. Graves' disease may have its onset after an external stressor In other instances, it may follow a viral infection or pregnancy. Many times the exact cause of Graves' disease is simply not known. It is not contagious, although it has been known to occur coincidentally between husbands and wives.
Signs and Symptoms

Hyperthyroidism may manifest as an enlarged thyroid (goiter), hair changes, erratic behavior, heart rate irregularities, tremor, sweating, palpitations, nervousness and increased activity and eye abnormalities.
The metabolic speed-up associated with hyperthyroidism is easily diagnosed in younger patients who present with symptoms of weight loss, excess appetite, sweating, rapid pulse and tremor. In older adults these characteristic symptoms may not exist. The elderly often present with depressed mood, confusion, heart failure, irregular pulse rate and a myriad of symptoms that do not readily suggest an acceleration of metabolism.
Diagnosis and Tests
Advances in laboratory technology now allow both underactive and overactive thyroid conditions to be diagnosed quickly and accurately with simple blood tests. Geriatricians routinely examine a patient's thyroid gland and order periodic blood checks – they believe it is best to detect and treat thyroid problems before significant symptoms arise. It is another reason why regular medical checkups are important for older adults.
Treatment and Prevention
Once diagnosed, treatment of hyperthyroidism in an older person is safely accomplished by administration of radioactive iodine. The zapped iodine molecules are taken up by the thyroid gland and tame the overactive factory.
The selection of treatment will include factors such as age, degree of illness, and personal preferences. Generally speaking, from least invasive to most invasive, the treatments include:
- Anti-thyroid drugs that inhibit production or conversion of the active thyroid hormone (20-30% effective, often used to control mild cases)
- Radioactive iodine (I-131), which destroys part or all of the thyroid gland and renders it incapable of overproducing thyroid hormone
- Surgery, in which most of the thyroid gland is removed, renders it incapable of overproducing thyroid hormone.
The latter two treatments result in a 90-95% remission rate of the disease. In a few cases the treatments must be repeated. In all cases lifetime follow-up laboratory studies must be done, and in almost all cases lifetime replacement thyroid hormone must be taken.
Prognosis; Complications
Grave's disease usually responds to treatment and, after the initial period of hyperthyroidism, is relatively easy to treat and manage.
Another common disorder of the thyroid gland is a nodule, or lump. A physician's main concern is whether the growth is caused by cancer. Fortunately, the vast majority of nodules discovered in the elderly are harmless. "Wait and watch" is usually the best advice. If cancer of the gland is discovered, the prognosis with treatment is usually good.
The more serious complications of prolonged, untreated, or improperly treated Grave's disease include weakened heart muscle leading to heart failure, osteoporosis, or possible severe emotional disorders.
Signs, symptoms & indicators of Hyperthyroidism:
Lab Values - Cells
Lab Values - Common
Lab Values - Hormones
Symptoms - Bowel Movements
Symptoms - Cardiovascular
Symptoms - Environment
Symptoms - Food - General
Symptoms - General
Symptoms - Head - Eyes/Ocular
Symptoms - Metabolic
Symptoms - Mind - Emotional
Symptoms - Mind - General
Symptoms - Muscular
Symptoms - Reproductive - Female Cycle
Symptoms - Reproductive - General
Symptoms - Skin - General
Symptoms - Sleep
Conditions that suggest Hyperthyroidism:
Circulation
 Megaloblastic Anemia / Pernicious Anemia
Megaloblastic Anemia / Pernicious Anemia
Hyperthyroidism is one of the minor causes of B12 deficiency.
Digestion
Glandular
Hormones
Male-Specific
 Male Infertility (Low Sperm Count)
Male Infertility (Low Sperm Count)
The thyroid gland is responsible for balancing cell metabolism, so when the thyroid gland is not functioning properly, cell metabolism suffers. This causes changes in the production of sperm.
Metabolic
Musculo-Skeletal
 Osteoporosis - Osteopenia
Osteoporosis - Osteopenia
Untreated hyperthyroidism accelerates bone resorption, reduces bone density, and over time increases the risk of osteoporosis.
Nervous System
Skin-Hair-Nails
Symptoms - Glandular
Risk factors for Hyperthyroidism:
Family History
Nutrients
 Copper Deficiency
Copper Deficiency
Although supportive data is limited, a report from a study group of hyperthyroid women suggests that copper status should at least be investigated in women with hyperthyroidism.
"Thyroid and immune system health are crucially dependent upon copper. As far as I can see now, copper deficiency is the most important factor in the development of hyperthyroidism. Virtually all hypers in the hyperthyroidism group have found that copper supplementation reduced their symptoms, usually within hours or a few days at most. Most have reported that within three to six months of beginning copper supplementation, they have been able to significantly reduce their intake of antithyroid drugs. While copper is the big story in hyperthyroidism, it is not the whole story. If it were, it would have been discovered years ago. Proper copper metabolism interrelates with and depends upon many other nutrients." [John Johnson, iThyroid.com]
 Iodine Requirement
Iodine Requirement
Hyperthyroidism may occur, particularly in elderly people, due to long term slight iodine deficiency as this may result in additional nodules on the thyroid.
Symptoms - Food - Intake
 High iodine consumption
High iodine consumption
Excessive iodine has a complex disruptive effect on the thyroid and may cause either hypothyroidism or hyperthyroidism in susceptible individuals.
Symptoms - Glandular
 History of hyperthyroidism
History of hyperthyroidism
Underlying hyperthyroidism often returns after antithyroid drugs are discontinued. For this reason, patients are often advised to consider a treatment that permanently prevents the thyroid gland from producing too much thyroid hormone.
Hyperthyroidism suggests the following may be present:
Addictions
 Cigarette Smoke Damage
Cigarette Smoke Damage
A study of 132 pairs of twins (264 subjects) showed that smoking can have negative effects on the endocrine system, causing a 3- to 5-fold increase in the risk of all types of thyroid disease. The association was most pronounced in autoimmune disorders (Graves' disease and autoimmune thyroiditis), although there was still a strong association for non-autoimmune thyroid disorders.
Autoimmune
 Autoimmune Tendency
Autoimmune Tendency
The leading cause of hyperthyroidism is Graves' disease, which is an autoimmune disorder.
Recommendations for Hyperthyroidism:
Diet
 Gluten-free Diet
Gluten-free Diet
Some doctors recommend the complete avoidance of gluten/gliadin and dairy products when this allergy is suspected in cases of Graves' disease or other autoimmune disease.
 Dairy Products Avoidance
Dairy Products Avoidance
One doctor reports that taking calcium without magnesium is one of the worst things you can do if you have hyperthyroidism because this increases any magnesium deficiency and increases the heart rate and likelihood of arrhythmia. This is one of the reasons why dairy products, which are high in calcium and low in magnesium, need to be restricted until magnesium levels are replenished.
Digestive Aids
 Hydrochloric Acid (Trial)
Hydrochloric Acid (Trial)
Some doctors report that 50% of patients with autoimmune disease are also hypochlorhydric.
Invasive / Surgery
 Neural Therapy
Neural Therapy
Neural Therapy to the thyroid gland may help normalize its function and stabilize or shrink nodules.
Laboratory Testing
 Test for DHEA
Test for DHEA
Some doctors report finding that a high percentage of patients with autoimmune disorders, such as Graves' disease, are also deficient in DHEA, and should be tested.
Mineral
 Iodine
Iodine
Very high doses of Iodine for short periods (about thirty drops daily of SSKI for three weeks) have sometimes produced favorable results in Graves' disease. Because of the possibility of causing a 'thyroid storm' (an acute hyperthyroid state), this therapy should only be attempted under close supervision by a doctor experienced in its use: Excessive iodine ingestion can cause either hypothyroidism or hyperthyroidism and should be avoided.
 Selenium
Selenium
A review of medical literature that focused on 69 articles published between 2000 and 2016 concluded that the maintenance of proper selenium levels in the body (not too high and not too low) is a prerequisite not only to prevent thyroid disease but also to maintain overall health. [Mara Ventura et al., Int J Endocrinol. 2017; 2017: art.1297658]
The thyroid gland contains the highest concentration of any organ in the body. Selenium is vital for the production of thyroid hormone and is involved in the conversion of T4 (inactive thyroid hormone) to T3 (the active form). Two important groups of enzymes within the thyroid are selenoproteins, which depend on selenium. Mercury and cadmium are major thyroid disruptors but not when sufficient selenium is available: selenium binds to mercury and makes it completely inert; it also binds to cadmium and facilitates its excretion through bile. Selenium and iodine are both essential for thyroid hormone production and a deficiency in either will cause problems.
On June 22, 2001 Dr. Barbara Gasnier reported the findings at the 83rd Annual Meeting of the Endocrine Society in Denver, Colorado that selenium supplementation may prevent progression of autoimmune thyroid disease, especially during the onset of the disease.
According to the researchers, selenium deficiency appears to contribute to the development and maintenance of autoimmune thyroiditis because of its effect on the function of selenium-dependent enzymes, which can modulate the immune system.
Selenium supplementation with 200mcg of sodium selenite may improve the inflammatory activity seen in patients with autoimmune thyroiditis, but whether this effect is specific for autoimmune thyroiditis or may also be effective in other organ-specific autoimmune diseases remains to be investigated. Selenium supplementation may lower free radical activity, which contributes to inflammation.
It appears that taking selenium without iodine will result in a decrease in production of Thyroxine (T4), although there may be an initial transient increase in T4 to T3 conversion and hence higher T3 and seemingly worse hyperthyroidism.
Click to see sample report
Your body is a highly complex, interconnected system. Instead of guessing at what might be wrong, let us help you discover what is really going on inside your body based on the many clues it is giving.
Our multiple symptom checker provides in-depth health analysis by The Analyst™ with full explanations, recommendations and (optionally) doctors available for case review and answering your specific questions.
KEY














