Peripheral Vascular Disease: Overview
Alternative names: PVD, Peripheral Artery Disease, Peripheral Arterial Disease, PAD, Leg Artery Disease
Peripheral Vascular Disease (PVD) refers to diseases of the arteries and veins that are located outside the heart and brain. It is a common circulatory problem in which narrowed arteries reduce blood flow to the limbs.
- let The Analyst™ find what's wrong
- understand what's happening to your body
- have a doctor review your case (optional)
When PVD develops, the body's extremities (usually the legs) receive insufficient blood to satisfy their needs, causing symptoms such as leg pain when walking.
Incidence; Causes and Development; Contributing Risk Factors
About 5% of people over the age of 50 are believed to suffer from peripheral artery disease. Peripheral artery disease is slightly more common in men than in women.
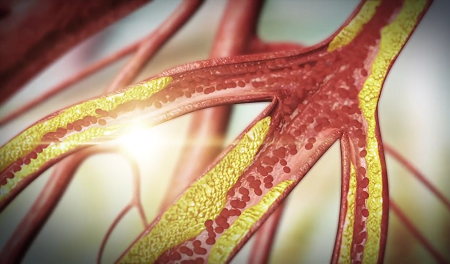
Peripheral artery disease is often caused by atherosclerosis. Although we usually think of the heart when discussing atherosclerosis, it can and usually does affect other arteries in the body as well; when it occurs in the arteries supplying blood to the limbs, it causes peripheral vascular disease.
A number of conditions such as vasculitis may cause damage to blood vessels throughout the body. Injuries to blood vessels (such as those occurring in a car accident or sports injury), blood-clotting disorders, and damage to blood vessels during surgery can also lead to tissue ischemia.
Other less common causes include blood vessel inflammation, injury to the limbs, unusual muscle or ligament anatomy, or radiation exposure.
Risk factors for peripheral vascular disease are similar to those for atherosclerosis and include:
- Smoking
- Diabetes mellitus (both type 1 and type 2 diabetes)
- Obesity (body mass index over 30)
- Physical inactivity
- Hypertension
- High LDL ("bad") cholesterol
- Low HDL ("good") cholesterol
- High levels of triglycerides
- Being over 50 years old
- A family history of peripheral vascular disease, hypertension, heart disease, atherosclerotic disease or stroke
- High homocysteine levels
- Chronic renal failure
The risk factors are additive, meaning that a person with a combination of two risk factors – diabetes and smoking, for example – has an increased likelihood of developing more severe peripheral artery disease than a person with only one risk factor.
Signs and Symptoms

Approximately half of people with PVD do not experience any symptoms, but for those with symptoms the most common is leg pain when walking (intermittent claudication). Symptoms of PVD depend upon the location and extent of the blocked arteries and include:
- Painful cramping in the hip, thigh or calf muscles after activity such as walking or climbing stairs (Intermittent claudication)
- Leg numbness or weakness of the calf muscle
- Atrophy of the calf muscle
- Coldness in the lower leg or foot, especially when compared with the other side
- Sores on the toes, feet or legs that won't heal (ulcers)
- A change in the color of the legs
- Feet turn pale when elevated, and dark red when lowered
- Hair loss or slower hair growth on the feet and legs
- Slower growth and/or thickening of the toenails
- Shiny skin on your legs
- No pulse or a weak pulse in your legs or feet
- Erectile dysfunction in men
- (In critical cases) Rest pain, which occurs when the artery occlusion is so severe that there is not enough blood and oxygen supply to the lower extremities even at rest. The pain typically affects the feet, is usually severe, and occurs at night when lying down.
As peripheral artery disease progresses, pain may occur even when at rest or when lying down, and it may be severe enough to disrupt sleep.
Diagnosis and Tests

Aside from visible signs of Peripheral Artery Disease, other signs include:
- weak or absent pulse in the extremities
- sounds (bruits) that can be heard with a stethoscope
- blood pressure changes in the limbs between rest and exercise (the treadmill test)
- pale, shiny, thin skin and nail changes due to tissue ischemia (inadequate blood supply)
Radiologic imaging techniques including Doppler ultrasound, Duplex ultrasound, and MRI angiography are used to help diagnose peripheral vascular disease.
Treatment and Prevention
Treatment goals include pain relief, improving exercise tolerance, and preventing critical artery occlusion, heart attacks and strokes.
Peripheral vascular disease can be successfully treated by lifestyle alterations, medications, angioplasty and related treatments, or surgery. Lifestyle alterations also help prevent PVD and include quitting tobacco, exercising and eating a healthy diet.
Smoking cessation eliminates a major risk factor for disease progression and lowers the incidences of rest pain and need for amputations. It also helps prevent heart attacks and strokes.
Properly supervised exercise can condition the muscles to use oxygen more effectively and improve circulation.
Medications may be required and include:
- Cholesterol-lowering drugs such as statins
- Medications such as cilostazol (Pletal) and pentoxifylline (Trental) which increase blood supply to the extremities
- Medications to control high blood pressure
- Antiplatelet medications such as aspirin and clopidogrel (Plavix) to reduce blood clotting
- Anticoagulant medications prevent blood clotting for those at risk. Examples are heparin and warfarin (Coumadin)
Other risk factors, such as diabetes, poor lipid levels, and high blood pressure should be reduced as far as is possible.
When experiencing pain while lying down, hanging your legs over the edge of your bed or walking around your room may temporarily relieve the pain.
Angioplasty is a nonsurgical procedure that can widen a narrowed or blocked arteries. In more difficult cases, surgical techniques such as bypass surgery (creating detours around a blocked artery) or endarterectomy (cleaning out plaque buildup inside an artery) can be used.
Seek medical attention if...
If you have leg pain, numbness or other symptoms, don't dismiss them as a normal part of aging – see your doctor.
On This Page
Peripheral Vascular Disease:Signs, symptoms & indicators of Peripheral Vascular Disease:
Symptoms - Skeletal
Conditions that suggest Peripheral Vascular Disease:
Circulation
 Intermittent Claudication
Intermittent Claudication
The first symptom of leg artery disease is usually pain in the legs that comes on after walking for a while and goes away with rest. This "angina of the legs" is called intermittent claudication. It is not a normal part of getting older. If you feel it, report it to a doctor.
Risk factors for Peripheral Vascular Disease:
Circulation
 Atherosclerosis
Atherosclerosis
Peripheral artery disease is a likely sign of more widespread accumulation of fatty deposits in your arteries: Atherosclerosis of the peripheral arteries is by far the most common cause of peripheral vascular disease.
Supplements, Medications, Drugs
 Much/some B-complex supplementation
Much/some B-complex supplementation
By reducing the level of homocysteine in the blood, and therefore the risk of atherosclerosis, the B vitamins also reduce the risk of developing conditions that can be caused by atherosclerosis, including peripheral vascular disease.
Click to see sample report
Your body is a highly complex, interconnected system. Instead of guessing at what might be wrong, let us help you discover what is really going on inside your body based on the many clues it is giving.
Our multiple symptom checker provides in-depth health analysis by The Analyst™ with full explanations, recommendations and (optionally) doctors available for case review and answering your specific questions.
KEY








