Poor Circulation: Overview
Good health and an active lifestyle depend on good circulation. That means a good flow of life-sustaining blood to every part of the body, from deep within organs like the heart and brain all the way out to the fingertips and toes.
- check your overall health status
- understand what's happening to your body
- identify any nutritional deficiencies
Unfortunately, the circulatory system, like the highway system of a great city, can become a bit the worse for wear after years of hard use. Congestion and traffic jams can afflict the arteries and veins, and "potholes" may even develop.
The body's circulatory system is like a two-part highway system. One set of roads leads out to the suburbs from the city center; the other leads back in.
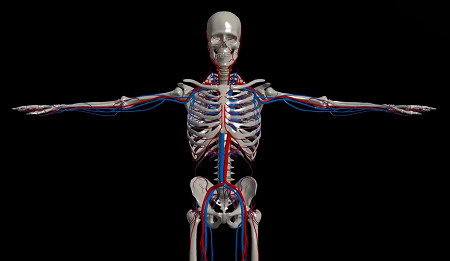
Arteries are the muscular vessels that carry blood to the outer reaches (the periphery) of the body. Arterial blood, freshly enriched with oxygen from the lungs and heart, is a bright red color.
Veins are the return network. Through them, blood travels back to the lungs and heart – an uphill trip against gravity from the legs and feet that uses a system of one-way valves. Blood in the veins has spent its oxygen load, and so appears bluish in color. At the periphery, these two highway systems are linked through a vast network of tiny back roads – little vessels called capillaries that do the work of delivering oxygen to the body's tissues.
Both sides of this blood delivery system can run into problems, especially in later life. With arteries, the problem is most likely to be narrowing or blockage by fatty deposits that cling to the inner walls of the vessels. With veins, swelling, inflammation, and clotting are the chief offenders.
The veins near the surface of the leg can become painfully inflamed in a condition called phlebitis. The inflamed vein may feel like a cord that is warm and tender to the touch. Aside from the risk of clot formation or infection, phlebitis isn't harmful, just uncomfortable.
Incidence; Causes and Development; Contributing Risk Factors
Peripheral Vascular Disease slows the pace of one million Americans each year, affecting more than 5% of those aged over 70.

Peripheral Vascular Disease. Almost everyone knows how atherosclerosis (hardening of the arteries) affects the heart. If an artery that supplies the heart muscle becomes partially blocked, it can cause angina (chest pain) when exercise puts extra demands on the heart. If the blockage is total, the result is a heart attack. But peripheral arteries (those distant from the heart, usually in the lower legs and feet) can become blocked, too.
The medical term for leg artery disease is peripheral vascular disease. The root causes are the same as for heart disease: Excess levels of fatty substances, including cholesterol, circulate in the bloodstream. Over many years, fatty deposits called plaque build up inside the vessels like rust in a pipe, narrowing the opening through which the blood must flow. At the same time, the walls of the arteries themselves can become roughened and stiff. Tiny clots may become snagged in these areas, reducing blood flow even further.
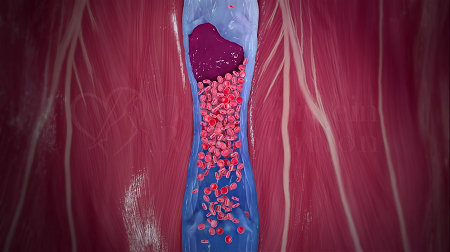
Vein Problems. Veins have the task of transporting blood from all over the body back up to the lungs for a breath of fresh air. These blue-looking vessels are thinner and less muscular than the arteries. They're also under far less pressure from the heartbeat. So, to keep the blood moving back toward the heart, they must rely on help from a series of small interior valves and the massaging action of surrounding muscles. If these helpers fail to do their job, blood can bog down in the outer reaches of the system; veins can swell and become irritated; and clots can form and travel to other parts of the body.
Varicose veins are the most visible vein problem, but not as serious as venous thrombosis – the formation of a blood clot in a vein deep within the tissues. The danger lies in the chance that such a clot could travel to the lungs, where it can cause a potentially fatal condition called a pulmonary embolism. (A blood clot in a vein near the surface of the body, as in varicose veins, rarely breaks free and causes trouble elsewhere.)
Circumstances that increase the chances of clot formation in the veins include:
- Sluggish blood flow in the arms and, especially, the legs, such as that caused by prolonged bed rest or sitting
- Damage to a vein's lining from infection, inflammation, or injury
- Conditions that cause blood to thicken or coagulate abnormally
Thrombosis usually strikes without warning, but there are some measures you can take to reduce your risk. Whenever possible, avoid prolonged periods of inactivity that allow blood to pool in your lower legs. On a long car or plane trip, take a walk-and-stretch break as often as possible. If you're laid up with the flu for a week or two, have someone help you move around a few times a day. These tactics are especially important if you have ever had any clotting problems in the past.
Signs and Symptoms
A deep-vein clot may cause no symptoms until it travels to the lungs, or it may cause pain and swelling in one leg.
Warning signs of Leg Artery Disease:
- Lower-leg pain that comes on with walking and subsides with rest
- Lower-leg pain that is worse when you are lying in bed at night or when legs are elevated
- Numbness or coldness of toes, feet, or lower legs
- Pale, hairless, mottled, scaly, or shiny skin on the calves, ankles, or feet
- Brittle toenails
- Lower-leg ulcers or hard-to-heal cuts and scratches
Diagnosis and Tests
To be certain of the problem, a complete diagnostic workup is required.
Treatment and Prevention

Effective treatments are available for many common circulatory problems. Clogged arteries can be opened and unsightly varicose veins can be removed. But prevention is by far the best strategy. Even later in life, relatively simple measures like a brisk daily walk and giving up cigarettes can often keep circulation problems at bay, or at least keep them from getting worse.
Therapy starts with an effort to determine why clotting is abnormal, and usually involves giving medications to reduce clotting and thin the blood.
If you experience venous thrombosis, you'll be prescribed bed rest for a while, with legs elevated. After the swelling goes down, a below-the-knee elastic stocking may be recommended, and you'll be told to avoid long periods on your feet. If you must take anticoagulant drugs, regular monitoring may be required to steer clear of bleeding problems.
Treatment of phlebitis consists of pain-relieving medications, such as NSAIDS, and warm compresses over veins. If clot formation starts and moves into the deeper veins, the situation could become dangerous, so prompt treatment is important.
Since the same process of plaque buildup underlies both heart disease and leg artery disease, it isn't surprising that preventive measures are very similar. Of course, everyone knows that not smoking, a low-fat diet, regular exercise, and control of high blood pressure and high blood cholesterol can help stave off a heart attack. But they can also prevent a "leg attack" every time you take a brisk stroll to the mailbox.
Quit smoking. Giving up cigarettes is absolutely essential to controlling leg artery disease. The various toxins in cigarette smoke don't just damage the lungs; they harm the heart and the arteries throughout the body as well. Given the strong association between smoking and leg artery problems, kicking the habit is essential to kicking up your heels as you grow older.
Feet with an inadequate blood supply are very susceptible to infections that can develop into ulcers or even gangrene. If you have poor circulation in the legs or feet, especially with diabetes:
- Wash feet daily with gentle soap and blot dry; then apply moisturizing lotion.
- Wear well-fitting, low-heeled, comfortable shoes that protect the feet and don't rub or bind. Avoid high heels and open-toed sandals.
- Keep feet dry; dampness can encourage fungal infections such as athlete's foot. Wear breathable wool or cotton socks, and treat fungal infections promptly.
- Trim toenails carefully, or have them professionally trimmed by a podiatrist, especially if they are thickened. Never cut corns or calluses or use drugstore remedies on them without approval of the doctor or podiatrist.
- Check feet frequently for small injuries or irritation, especially if you have poor sensation in the feet or toes. Don't let small problems turn into large ones.
Keep moving! If leg artery disease is causing you discomfort, you may not feel like walking; but hang in there anyway. Take a brisk walk for a half-hour to an hour – preferably each day, but at least three times a week. Experts aren't sure just why walking helps improve the condition, but they know it does. It may encourage the development of tiny "detours" (called collateral circulation) through unblocked vessels, or it may just train leg muscles to use oxygen more efficiently.
In any case, get moving: Walk until the discomfort sets in, then slow down or stop. Once pain subsides, resume your pace. Don't try to walk "through" severe pain. In winter, indoor exercise may be a better bet, since claudication pain can be triggered or worsened by cold. Mall-walking, exercise bicycles, or treadmills are possibilities. Start swimming in an indoor pool, or just walk in the water, backward as well as forward. It's likely you'll start to feel a difference before long – and such a program of regular exercise has many other benefits, too. It burns calories, keeps you limber, and lifts your spirits.
Keep tabs on blood cholesterol. If you are diagnosed with leg artery disease, it's a good bet that your blood cholesterol levels are too high. If you don't know your cholesterol numbers yet, ask your doctor to measure your levels of "good" (HDL) and "bad" (LDL) cholesterol. If you find you do have a significant blood cholesterol problem, it's never too late to start treatment, which will reduce your risk of heart disease, as well.
Trim dietary fat. This is good advice for everyone, and since most people with leg artery disease have too much blood cholesterol, it makes extra good sense for them. A lean diet can help lower blood fats that circulate throughout the body.
Keep high blood pressure under control. Elevated pressure within the arteries causes long-term damage to the vessels themselves and the organs they supply. If you have high blood pressure, keep it at normal levels through diet, exercise, and prescribed medication. This will yield fringe benefits for the entire circulatory system.
Heads up at night. If you have resting pain in bed at night, try sleeping with a wedge-shaped pillow to elevate your head and upper body. That helps gravity send blood down to your feet.
Leg artery disease is not easily managed by simply popping a pill.
Prognosis; Complications
You may have seen warnings that circulatory problems, if left untreated, can result in tissue damage, eventually leading to ulcerations, gangrene, and even amputation. That's true. However, dire complications such as these can almost always be prevented by prompt, careful medical attention. And taking care of circulatory problems can yield positive results as well: Peak circulation lets you enjoy all your favorite activities, whether you prefer golf, tennis, or just a walk around the mall.
Vein trouble, especially if left untreated, can result in chronic swelling, aching, and tiredness in the legs. Over time, the ankles and lower legs may take on a dark reddish tone with skin problems and even leg ulcers.
Trapped in quiet backwaters along the circulatory system in the legs, undisturbed blood can settle and form clots. Chances of the phenomenon increase when prolonged inactivity slows the flow of blood to a crawl. If a clot breaks free and travels to the lungs, the results can be fatal; so it's very important to keep your legs moving, even when confined to bed. By tightening the veins and thus speeding the flow of blood, elastic stockings often help too.
On This Page
Poor Circulation:Conditions that suggest Poor Circulation:
Circulation
Metabolic
Risk factors for Poor Circulation:
Addictions
Circulation
 Coronary Disease / Heart Attack
Coronary Disease / Heart Attack
Not everyone with heart disease gets peripheral vascular disease, and vice versa. For some reason, the process of atherosclerosis seems to affect different people in different places. However, if you have one, you are definitely at increased risk for the other.
Habits
Lab Values
Organ Health
 Diabetes Type II
Diabetes Type II
Up to 50% of all people with leg artery disease have diabetes; for them, controlling both conditions is crucial. Diabetes increases your risk for leg artery disease fourfold, and accounts for nearly half of all amputations in the U.S. that aren't related to accidents.
Diabetes makes hardening of the arteries much more dangerous (especially in the feet and toes) through several different mechanisms, and it's still not fully understood which ones matter most. People with diabetes are prone to nerve damage in the legs and feet, which means they often may overlook minor injuries. This, combined with poor circulation that slows wound healing, can cause small wounds to develop into more serious infections. Diabetes also makes people more likely to develop blockages in smaller vessels far from the heart, and those blockages tend to be more widespread and harder to treat.
Poor Circulation can lead to:
Circulation
 Cold Hands and Feet
Cold Hands and Feet
In cases of peripheral vascular disease, the arteries narrow and there is a marked reduction of blood flow especially to the fingers and toes.
Recommendations for Poor Circulation:
Invasive / Surgery
 Surgery
Surgery
Many severe blockages in the heart or elsewhere can now be cleared away without surgery, and surgery isn't for everyone: It is expensive and involves at least some degree of risk from infection, clotting, and other complications. Also, those freshly opened arteries may well close up again with the passage of time.
When surgery is the only answer, there are two major options. In a bypass operation, the surgeon grafts a segment taken from one of the patient's veins (or sometimes an artificial vessel) onto the clogged artery, giving blood a pathway around the blockage. Alternatively, the surgeon can open the vessel and cut the plaque away (a procedure called endarterectomy).
Laboratory Testing
Click to see sample report
Your body is a highly complex, interconnected system. Instead of guessing at what might be wrong, let us help you discover what is really going on inside your body based on the many clues it is giving.
Our multiple symptom checker provides in-depth health analysis by The Analyst™ with full explanations, recommendations and (optionally) doctors available for case review and answering your specific questions.
KEY










