Iron Deficiency Anemia: Overview
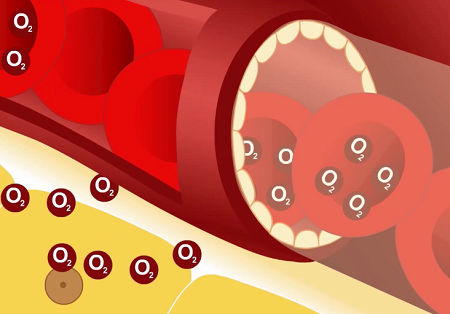
Iron deficiency anemia is the most common form of anemia. Iron is an essential component of the hemoglobin molecule: without iron the bone marrow is unable to produce hemoglobin. The red cell count falls and those which do enter circulation are smaller than normal (microcytic) and lacking in hemoglobin, hence they are pale (hypochromic).
- check your overall health status
- learn what you should be doing right now
- identify any nutritional deficiencies
The deficiency of iron may be absolute (there is no iron available for the production of hemoglobin – this is true iron deficiency anemia) or relative (the iron is present in storage in the marrow but other reasons prevent its incorporation into red blood cells).
Causes and Development
The average amount of iron in the average adult male is 4gm and in the average adult female 2.5gm. The normal North American diet contains approximately 15-20mg of iron per day. Most is present in meat and green vegetables; approximately 1.0mg is absorbed each day and just about an equal amount is lost in feces and sweat. As a result, the average adult's iron intake is in delicate balance, but is of little consequence as there is slightly more iron absorbed than lost and a store of iron is gradually accumulated. If, for some reason, the rate of iron loss increases, these stores can be depleted and an absolute iron deficiency develops. Such a deficiency requires large doses of supplemental iron to resupply the body stores and sufficient monitoring to prevent iron overload.
Causes of iron deficiency include:
- Diet – uncommon except in children
- Failure to absorb
- Increased utilization (for example pregnancy, adolescent growth)
- Atransferrinemia
- Failure to utilize (for example lead poisoning, chronic diseases)
- Blood loss.
Chronic blood loss is the most common cause of iron deficiency anemia. It must be remembered that anemia in iron deficiency develops slowly. The type and severity of the anemia varies with time. The development stages are:
- Depletion of iron stores, decreased ferritin levels, no anemia
- Increased transferrin levels, no anemia
- Fall in serum iron, no anemia
- Development of normocytic, normochromic anemia
- Development of microcytic, hypochromic anemia.
Signs and Symptoms
Along with those mentioned below, symptoms often include malaise (a vague feeling of physical discomfort or uneasiness).
Diagnosis and Tests
Laboratory Diagnosis of Iron Deficiency
Routine procedures. Hgb, Hct and RBC count are all decreased. The degree of decrease depends upon the length of time the marrow has been without sufficient supplies of iron. Because marrow can continue to produce empty cells, the red cell number will not be proportionately as low as the Hgb and Hct values. Serum ferritin is a better measure of body iron stores than any value in the complete blood count, as it will begin dropping long before other signs appear in the blood.
Indices. MCV – decreased, MCH – decreased, MCHC – decreased. The MCHC is the last to become lowered because as the marrow becomes more and more depleted of iron it produces smaller cells with a smaller amount of hemoglobin in each in an attempt to keep the concentration of hemoglobin in each normal. The RDW is increased, reflecting the anisocytosis characteristic of iron deficiency.
Treatment and Prevention
Treatment depends on the underlying cause. Iron deficiency anemia is usually easy to resolve; an anemia that does not respond as expected may require the help of a hematologist and additional testing.
On This Page
Iron Deficiency Anemia:Signs, symptoms & indicators of Iron Deficiency Anemia:
Lab Values - Cells
Lab Values - Chemistries
 Elevated TIBC
Elevated TIBC
While TIBC is commonly elevated in cases of iron deficiency anemia, it is also increased through the use of oral contraceptives and in pregnancy, blood loss and acute liver damage.
Symptoms - Bowel Movements
Symptoms - Environment
Symptoms - Head - Eyes/Ocular
Symptoms - Metabolic
Symptoms - Nails
Conditions that suggest Iron Deficiency Anemia:
Dental / Oral
Mental
Sleep
Symptoms - Cardiovascular
Risk factors for Iron Deficiency Anemia:
Autoimmune
 Gluten Sensitivity / Celiac Disease
Gluten Sensitivity / Celiac Disease
Anemia is a frequent presentation of celiac disease. In one study, 200 consecutive patients of a hematology clinic were screened for antigliadin and antiendomysial antibodies. Patients with both positive titers underwent intestinal biopsy, and in 10 patients (5%), results were positive for celiac disease. The prevalence increased to 8.5% if the patients with macrocytic anemia and the patients with bleeding who responded to iron therapy were excluded.
Digestion
 Gastrointestinal Bleeding
Gastrointestinal Bleeding
People with long-term bleeding that tends to occur in small amounts or intermittently may develop symptoms of anemia, such as tiring easily and looking unnaturally pale.
Nutrients
 Copper Deficiency
Copper Deficiency
Copper deficiency, due to its effects on ceruloplasmin, may cause an iron-deficiency anemia which can only be corrected with copper supplementation as it impairs iron absorption, reduces heme synthesis and increases iron accumulation in storage tissues. [J Orthomol Med 4( 2): pp.99-108, 1989]
Symptoms - Reproductive - General
Tumors, Benign
Recommendations for Iron Deficiency Anemia:
Botanical / Herbal
Diet
 Caffeine/Coffee Avoidance
Caffeine/Coffee Avoidance
Research has shown that drinking coffee causes a significant loss of several vitamins and minerals, including vitamins B and C, calcium, iron, and zinc.
Homeopathy
Laboratory Testing
Mineral
 Iron
Iron
Iron supplementation, with as much as 200mg of elemental iron per day, is the obvious therapy for treating and preventing the recurrence of iron deficiency anemia. Note, however, that it is dangerous to take iron supplements without first having ferritin levels tested, as taking iron when it is not called for can cause iron overload disorder, potentially a dangerous condition.
 Molybdenum
Molybdenum
Molybdenum may help prevent anemia by helping mobilize iron, provided there are sufficient iron stores.
Vitamins
 Vitamin C (Ascorbic Acid)
Vitamin C (Ascorbic Acid)
It has been well established that better iron absorption occurs from both plant and animal sources when vitamin C is taken at the same time, whether from foods or as a supplement. 75mg of vitamin C in a meal will cause about a six-fold increase in the absorption of heme iron. It appears that vitamin C enhances non-heme iron absorption in individuals with low iron status, but does not increase iron status unnecessarily in iron-replete individuals. [Effect of ascorbic acid on iron absorption from different types of meals. Hum Nutr: Appl Nutr,1986 40A: pp.97-113]
Click to see sample report
Your body is a highly complex, interconnected system. Instead of guessing at what might be wrong, let us help you discover what is really going on inside your body based on the many clues it is giving.
Our multiple symptom checker provides in-depth health analysis by The Analyst™ with full explanations, recommendations and (optionally) doctors available for case review and answering your specific questions.
KEY














